‘Measuring the size of a fist and located in your lower back, the kidneys are a hive of activity. Find out more about what kidneys do and what is kidney disease?’
What do kidneys do and what is kidney disease?
The kidneys are two bean shaped organs located in your lower back. Each kidney is about the size of a fist and weighs about 4-6oz. Inside the kidneys are tiny structural and functional units call nephrons which filter the blood.
The kidneys have many functions, including:
- Removal of wastes and excess fluids by cleaning and filtering the blood, and producing urine.
- Production of hormones which help maintain healthy bones, control blood pressure and control the production of red blood cells which carry oxygen around the body.
What is kidney failure?
Kidney failure may be described as a loss in the kidney’s ability to filter (remove) waste products from your blood. Kidney failure can happen quickly, caused by for example a sudden loss of large amounts of blood, or an accident and this is called acute kidney injury. Acute Kidney Injury is usually short lived, but can occasionally lead to lasting kidney damage. It may also be abbreviated to AKI.
More commonly, kidney function worsens over a number of years and this is called chronic kidney failure or chronic kidney disease (often abbreviated as CKD).The National Kidney Foundation state that up to two thirds of CKD is caused by uncontrolled diabetes or high blood pressure (hypertension). CKD is usually not reversible but if found early, progression can be delayed through medication, diet and lifestyle changes by maintaining current kidney function.
What is the definition of chronic kidney disease (CKD)?
Chronic kidney disease (CKD) is defined as the presence of kidney damage, or a decreased level of kidney function, for a period of three months or more.
Signs of kidney damage include:
- Persistent small and large proteins in the urine (proteinuria and microalbuminuria)
- Persistent blood in the urine (haematuria) – after exclusion of other causes, e.g. urological disease.
- Structural abnormalities of the kidneys demonstrated on ultrasound scanning or other radiological tests e.g. polycystic kidney disease, reflux nephropathy
- Biopsy proven chronic glomerulonephritis
The Irish Nephrology Society currently recommends classifying Chronic Kidney Disease into five stages based on a measure estimated glomerular filtration rate (eGFR).
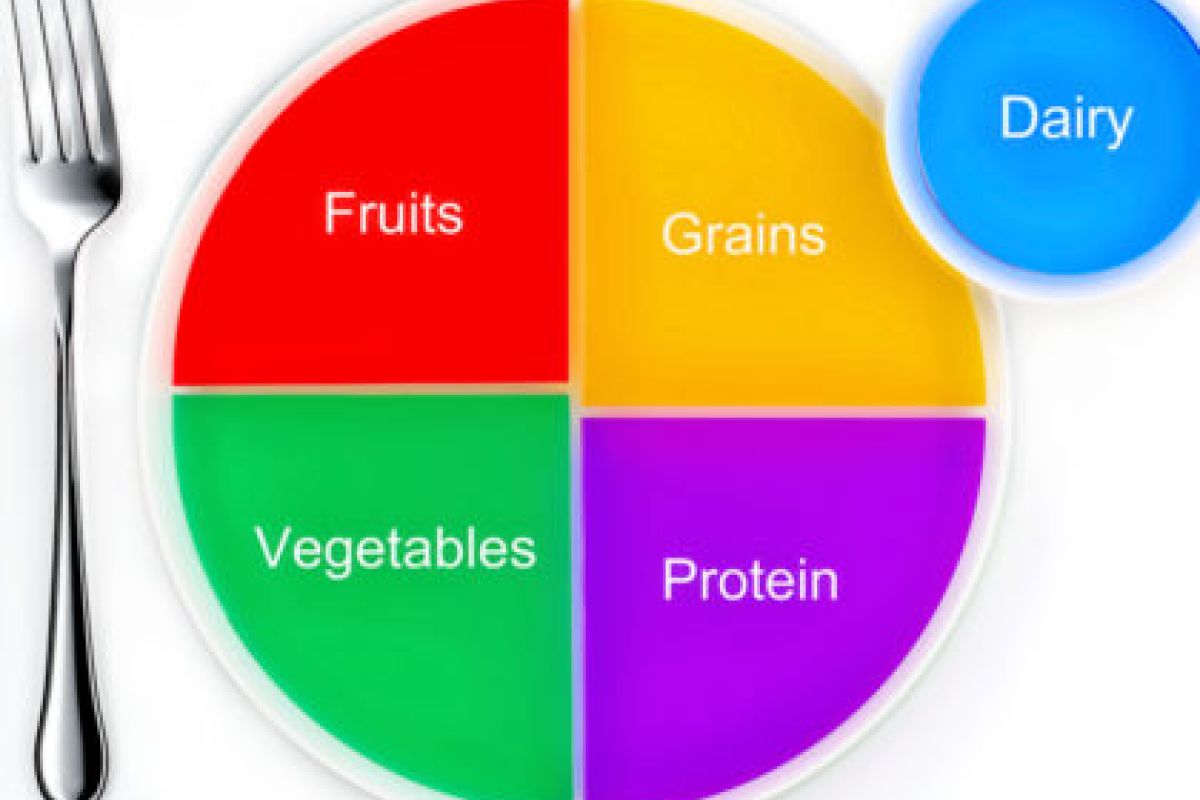
Sometimes CKD can lead to end stage kidney disease, (eFGR)(ESKD) which requires dialysis or a transplant to keep you alive. However, as the Irish Nephrology Society (INS) state, ‘the vast majority of patients with mild to moderate CKD will not require dialysis and can be managed in primary care’. Early detection and treatment may help prevent ESKD and the need for dialysis or transplant treatment. The kidney diet is one of the cornerstones of the treatment of CKD and helps with the target of delaying progression. The kidney diet is also essential in maintaining quality of life and functional capacity in people with kidney disease. The type of kidney diet required is individualised to the stage of kidney disease (based on eGFR), other diseases present (co-morbidities), the person’s age, weight and social situation. Some examples of important kidney diet changes in the early stages of CKD are ‘A No Added Salt’, ‘Weight Reduction’ (if overweight) and ‘Moderate Protein Intake’. A Kidney (Renal) Dietitian can assess your diet needs and advise on a tailor made kidney (renal) diet.
How do I know if I have CKD?
Chronic kidney disease includes conditions that damage your kidneys and decrease their ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, wastes can build to high levels in your blood and make you feel sick. You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. is sometimes called a silent disease because there are often no warning signs. Some signs of CKD are:
- Weight loss and poor appetite
- Swollen ankles, feet or hands (due to water retention)
- Shortness of breath
- Blood or protein in your urine
- An increased need to pass urine, particularly at night
- Itchy skin
- Muscle Cramps
- High blood pressure (hypertension)
- Nausea
- Erectile Dysfunction in men.
You often will not know if you have CKD as you may not experience any symptoms, however screening is based on simple urine and blood test that your doctor can easily perform. If you have high blood pressure or diabetes or you are obese, yearly screening should be considered with your doctor.
Remember! Early detection of CKD may allow you to delay progression through diet and lifestyle changes and medication.