Protein to build
‘Dietary protein in adequate amounts is required for normal body function, growth and repair but too much is not recommended in Chronic Kidney Disease. Here the Kidney (Renal) Dietitians explain about protein needs & the kidney diet’
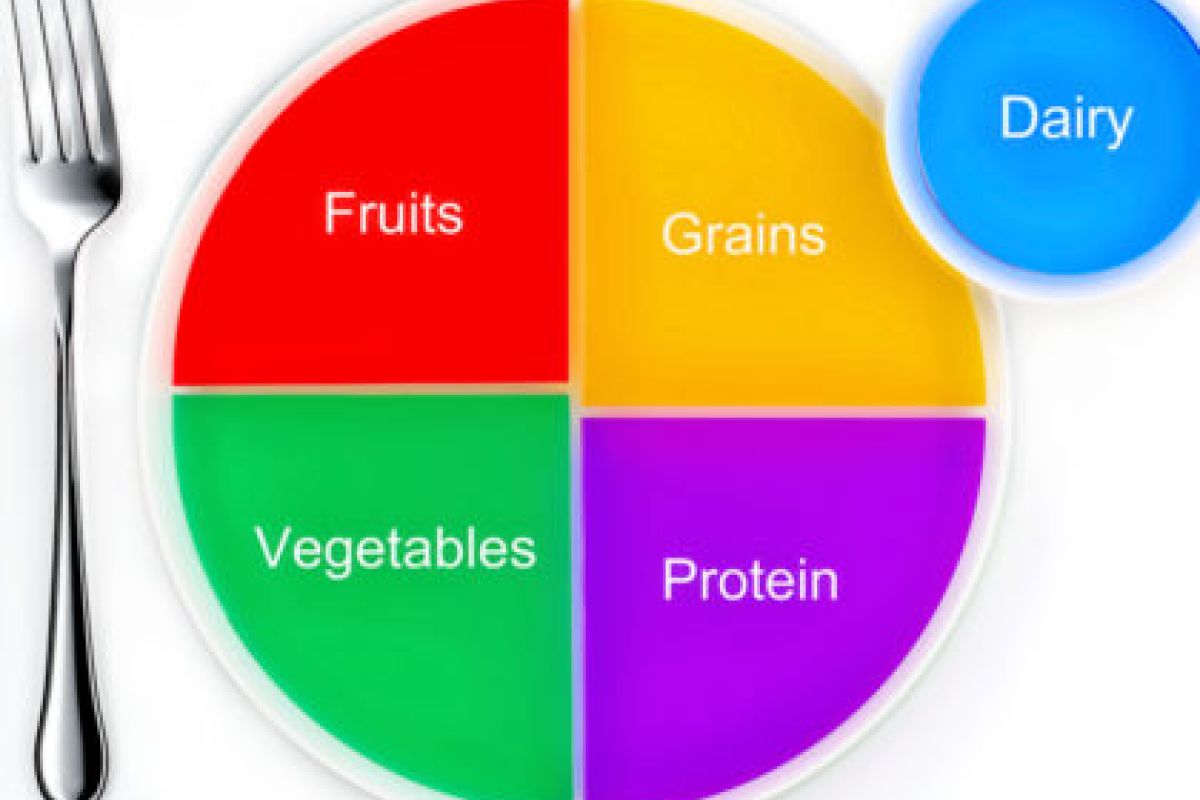
Dietary protein is important for normal function, growth and repair in all parts of the body, including the skin, muscles, blood and internal organs. Meat, fish, chicken, eggs and milk are foods rich in protein. Other foods, such as bread, pasta, rice and potatoes also contain protein in smaller amounts.
How much protein do I need to eat in my Kidney (Renal) diet?
The amount of protein you need depends on your stage of kidney disease, your size and whether or not you are on dialysis. Most people with kidney disease who are not on dialysis need to eat a moderate amount of protein. Your Kidney (Renal) Dietitian will give you a daily protein allowance and discuss with you how you can make small changes to your Kidney (Renal) diet to achieve this. Your Dietitian may guide you to estimate a serving or portion of protein as follows:
1oz cooked meat = a small matchbox size
3oz cooked meat = a deck of playing cards or average sized adult palm
Dietary Protein and Dialysis
When people start dialysis, they are usually advised to increase the protein they eat in their kidney diet. This is because a small amount of protein is lost with each dialysis session.
What happens if I get too much or too little protein in my kidney diet?
Eating too little protein can cause:
* Muscle Weakness
* Fluid Retention / Swelling at the ankles
* Poor health
* You to lose muscle instead of fat stores
Eating too much protein can cause:
* Nausea and Vomiting
* High levels of urea
* Loss of Appetite
* Fatigue
You may need more protein if you have an infection, or a wound to heal. If you cannot meet your protein needs with food alone, you may require a protein supplement. It is important to discuss this option with your Kidney (Renal) Dietitian before commencing any supplements.
Blood tests and Protein
Albumin is a type of protein found in the blood. It can be used to evaluate your nutritional status. A low albumin on your blood test can mean that you are not getting enough protein in your kidney diet. You should discuss this with your Kidney (Renal) Dietitian.
Phosphate Binders and Dietary Protein
If you have been prescribed a medicine called a phosphate binder, remember to take your binders as prescribed, as all foods that are high in protein are also high in phosphate.