Body Weight – Why watch it?
Written by Eamon Donovan on . Posted in Blog.
For those with CKD, achieving and maintaining a healthy body weight has many benefits including:
- Improved shortness of breath
- Relief for back and joint pain
- Confidence about body shape/ image
- Helping to prevent/ control high blood pressure & diabetes
- If a kidney transplant is a posibility, a healthy body weight is important for a successful transplant
Take Control of your weight.
REMEMBER this is only a guide. Your dietitian/ doctor can advise on what YOUR individual weight target should be. We are all very different with different dietary needs.
The renal dietary guidelines vary depending on your kidney function and the type of treatment you are receiving.
If you are trying to lose weight, or if you are trying to maintain an already healthy weight, here are a few tips to help you along the way.
Tips for getting started…
Tip 1: Have regular meals everyday starting with breakfast; avoid missing meals or eating late at night. If you are receiving dialysis, try to ensure you still eat regularly on the dialysis days.
Tip 2: Base your meal on starchy carbohydrate, choosing high fibre varieties e.g. wholemeal or wholegrain (speak to the dietitian if unsure of suitable choices). These will help you feel full up for longer; e.g. bread, potatoes, rice, pasta, cereals and noodles.
Tip 3: Eat fruit and vegetables within your dietary allowance, these are a healthy snack.
Tip 4: Avoid sugary drinks and sugar (added in drinks or on cereal). Use the low calorie varieties e.g. diet, low cal, sugar free. Artificial sweeteners can be used if required.
Tip 5: Choose low fat products where possible e.g. cheese, yoghurts (within allowances), low fat spread, low fat milk, salad dressings.
Tip 6: Fats and oils are very concentrated sources of calories, try not to fry food – grill, boil, or oven bake instead.
Tip 7: Control your portions/ fluid by using a small plate, cup, glass.
Tip 8: Set a realistic target, average recommended weight loss is ½ -1kg (1-2lbs) per week – weigh yourself only once each week at the same time, as your weight can fluctuate daily.
Tip 9: Avoid salt and salty foods to help protect the kidneys.
Tip 10: Sit down to eat at a table, eat slowly, chew well and enjoy your food. Eating in front of the television is a distraction and will leave you feeling less satisfied.
Tip 11: It is your daily routine that is important, special occasions can still be enjoyed. There may be times when you eat too much or make the wrong food choices, don’t let this stop you achieving your goal.
Tip 12: Never go shopping on an empty stomach, shop from a list.
Finally: Think long term, not quick fix. If you are following dietary advice for your kidney health be aware of this when trying to make suitable choices for weight loss or to when trying maintain a healthy weight.
With thanks to Briege O’ Kane, Senior Dietitian Renal, Letterkenny University Hospital, Letterkenny, Co. Donegal. On behalf of the Renal Interest Group of the Irish Nutrition and Dietetics Institute.
Treatment of hypoglycaemia (low blood sugar level)
Written by Eamon Donovan on . Posted in Blog.
IMPORTANT NOTICE:
The nutritional content of Lucozade Energy is changing…
The carbohydrate content of Lucozade Energy is being reduced by approximately 50%. Therefore if you use lucozade to manage your low blood sugar levels, you will need to take increase the amount of Lucozade you take.
From April 2017, the new Lucozade bottles and cans will be available. For a period of time, both old and new versions may be on the shelves together. It is therefore important that you remember to check the label for the amount of carbohydrate it contains.
To correct a hypo (low blood sugar level) you need to take 15g of rapidly absorbed carbohydrate. The new Lucozade product contains 8.9g carbohydrate per 100mls. Therefore you will now need to take 170mls to get 15g of carbohydrate to correct your hypo.
It is important to check labels regularly to ensure you are getting the right amount of carbohydrate as other brands of fizzy drinks may also change their sugar content
Barbara Gillman, Clinical Specialist Renal Dietitian, Mater Misercordiae University Hospital
Prepare Your Stock Cupboard For Winter
Written by Eamon Donovan on . Posted in Blog.
From Storm Abigail to Katie, the tumultuous winter weather and the chaos it causes can make access to Kidney friendly meal options more difficult. In 2016, Storm Barney left twenty five thousand people without power, roads were blocked and there was a status yellow Met Eireann wind warning advising us all to stay indoors.
This reminded me of the importance of having a well stocked food cupboard for winter with suitable no cook staples for those occasions when you have no electricity and sufficient non perishables and perishable items if you are confined to your house due to the weather.
With many stock cupboard items such as packet soup and tinned beans off the menu for those who need to watch salt, potassium and phosphate intake, some careful planning is required to stock your cupboard whilst sticking to your kidney (renal) diet. Some more suitable stock cupboard items are detailed in the table below. Utilising the Scout motto of Bi Ullamh (Be Prepared), winter storms will not hinder your ability to stick to your kidney diet.
In the Press |
In the Fridge & Freezer |
|
|
Some light meal ideas
1) Scrambled Egg and Toast 2) Tuna and mayonnaise sandwich 3) Creamy salmon and pasta (a small amount of melted cream cheese makes the sauce) 4) Porridge with tinned mandarins 5) Poached egg with Cajun pepper on toast 6) Crackers served with cream cheese and cucumber
|
|
Theresa Rennick, Senior Dietitian in Nephrology, (Midland Regional Hospital at Tullamore)
What Bread Can I Eat on a Renal Diet?
Written by Eamon Donovan on . Posted in Blog.
Bread type allowed on a renal diet can be a source of confusion for people with kidney disease. When we eat food our body uses what it needs and turns the rest into waste products. Bread is one of our staple foods and provides us with energy.
However, bread also contains some salt and phosphate. When your kidneys are not working properly, waste products like phosphate can build up in the blood. The kidneys can also find it more difficult to manage your blood pressure. The tables show the effects of too much salt and phosphate in our blood.
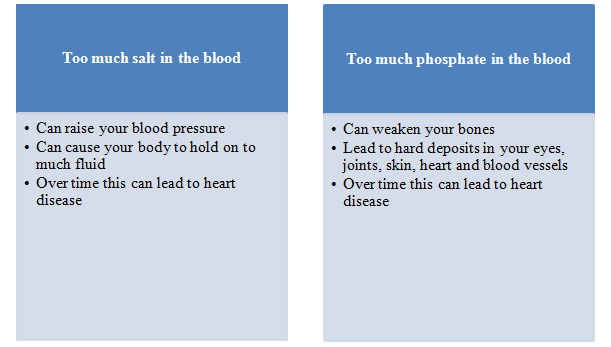
Salt (Sodium)
Most patients with kidney disease require a salt restriction. Salt is the main preservative used to keep our bread fresh. Breads can contain different amounts of salt per slice. Check food labels and try to pick one with lowest salt content.
If you are trying to gain weight or reduce your weight, please discuss with your dietitian how many slices of bread you should eat in the day.
Phosphate
As kidney function declines, so does the kidney’s ability to filter phosphate. Excess phosphate in the blood can cause problems with your heart and bones. White bread is lower in phosphate than brown bread. Often wholemeal or wholegrain sliced pan is also suitable for people on a renal diet (discuss what bread is suitable for you with your dietitian). Homemade soda bread (made without bran, wheatgerm, phosphate containing raising agent or baking powder) is also suitable but remember to count the milk, please see below for further advice on suitable bread types. Shop bought bread may not be suitable.
Diet sheet says: Sliced pan, baguettes, rolls, ciabatta, pitta bread, wraps;
choose wholemeal or wholegrain varieties;
homemade soda bread (count the milk)
Phosphate Food Additives
Manufacturers may add phosphorus when processing foods to thicken, improve taste or prevent discoloration. Added phosphate is very easily absorbed by the body. Dozens of additives contain phosphorus. Look for any ingredient that contains “phos” in the term. Here are some examples:
- Calcium phosphate
- Disodium phosphate
- Phosphoric acid
- Tricalcium phosphate
- Monopotassium phosphate
- Pyrophosphate polyphosphates
It is recommended that foods containing these additives are not eaten.
So what type of bread can I eat if I am on a low sodium and low phosphate diet?
Suitable bread types
White or brown pan loaf, baguettes, pitta bread, ciabatta, chapattis, white or granary bread rolls are all suitable. Your dietitian will decide if you can eat wholemeal bread based on your blood levels. Sourdough bread is not a suitable bread as it is high in phosphate. Your dietitian will also guide you on how many slices you should eat per day.
Homemade soda bread can be eaten once you discuss your phosphate and parathyroid hormone levels with your dietitian. Your recipe will also need to be reviewed by the dietitian so that milk used in making the soda bread can be incorporated into your daily dairy product allowance. Shop bought soda bread may also be suitable to eat if it contains no high phosphate containing ingredients such as baking powder, phosphate additives, bran or wheatgerm. Check the label for these ingredients or ask your baker. Ask you dietitian how much milk a slice of soda bread typically contains and count within your daily dairy product allowance.
Article Prepared by Barbara Gillman
Clinical Specialist Renal Dietitian, Mater Misericordiae University Hospital
On behalf of the Renal Interest Group, of the Irish Nutrition and Dietetic Institute
Lunch box treats
Written by Eamon Donovan on . Posted in Blog.
Why not brighten up these Autumn days with a lunch box treat?
We can all find it difficult to come up with new sandwich fillers and this can be more of a challenge when you trying to stick to your kidney friendly diet. Here are a couple of suggestions which will use up Sunday lunch leftovers and hopefully brighten up Mondays lunch box for the whole family.
Each recipe will tell you how many protein exchanges, as well as how many portions of fruit, vegetable, it provides per serving. All coding is based on one serving and not the full recipe. Check your diet sheet to see what your allowances are.
All the recipes are kidney friendly and do not include ingredients that are high in potassium, phosphate or salt. If they are low in fat they have been marked low fat. The coding system, which is based on the Irish Nutrition & Dietetic Institute (INDI) renal diet sheet, was developed for the Truly Tasty Cook book by Valerie Twomey.
Beef & Radish Salad Sandwich
Serves: 4
Ingredients:
2oz sour cream
4 medium red radishes, trimmed and thinly sliced
¼ teaspoon of white wine vinegar
½ teaspoon of pepper
3 dashes of Tabasco sauce
8 slices of white bread
Mixed salad leaves
8 oz of leftover roast beef
Directions:
- In a small bowl, mix the sour cream, radishes, vinegar, pepper and Tabasco sauce.
- On 4 slices of bread, layer a small handful of mixed salad greens, 2 oz of roast beef and the radish salad. Top each with another slice of bread and serve.
Per portion this dish provides: 319 kcal, 1 portion of vegetables and 2 protein exchanges.
Chicken and marinated courgette sandwich
Serves: 5
Ingredients:
150 g courgette
¼ red onion, thinly sliced
1 tablespoon thinly sliced lemon zest
2 tablespoon fresh lemon juice
2 tablespoon olive oil
Pepper
15 oz of roast chicken or chicken breasts
Handful of fresh parsley
5 crusty white rolls
Romaine lettuce
Directions:
- Slice the courgette into ribbons with a vegetable peeler. Combine with the red onion, lemon zest, lemon juice, olive oil and a pinch of pepper. Let stand for 30 minutes.
- Meanwhile roast the chicken breast or use leftover roast chicken. Let cool, then shred and add to the marinated courgette along with a handful of fresh parsley. Split the bread rolls, put a leaf of lettuce in each and then divide the chicken mixture, including the juice, between the 5 sandwiches. Enjoy!
Per portion this dish provides: 315 kcal, 1 portion of vegetables and 3 protein exchanges.
Blackberry and apple flapjacks
Serves: 12
Ingredients:
120g butter
80g demerera sugar
2 tbsp golden syrup
125g rolled oats
125g jumbo oats
250g bramley apple, peeled and grated
250g blackberries, washed
Instructions:
- Preheat the oven to 180c/gas mark 5.
- Melt the butter, sugar and golden syrup in a saucepan over a medium heat.
- When melted, remove from the heat, add the oats and grated apple and mix well.
- Grease a 20cm square cake tin and line with baking parchment (this makes it easier to get the flapjack out when it’s cooked).
- Press half the flapjack mix into the base of the tin, tumble the blackberries over the top and top with the rest of the flapjack so the blackberries are sandwiched in the middle. Press down slightly to stick all the layers together.
- Bake in the centre of the oven for 25-30 minutes until nicely browned. This flapjack may take longer to cook than normal flapjack due to the moistness of the added fruit, it will also remain moist when cool.
Per portion this dish provides: 204 kcal, ½ portion of fruit.
Oonagh Deeney. Senior Renal Dietitian, Beaumont Hospital
Spring time treats!
Written by Eamon Donovan on . Posted in Blog.
Why not celebrate the arrival of Spring with this tasty seasonal recipe for all the family.
Roast Lamb with Garlic & Country Herbs
Serves 12
Ingredients:

- 1 leg of lamb (2.5kg) trimmed
- 1 onion (240g) roughly chopped
- 125ml (¼ pt) water
Topping
- 2 large cloves of garlic (6g) peeled
- 2 dessertspoon root ginger (5g) chopped
- Grated rind of a small lemon
- 2 tablespoon fresh parsley (8g) chopped
- 2 tablespoon fresh mint (30g) chopped
- 1 tablespoon fresh rosemary (2g) chopped
- 1-2 tablespoon olive oil
To Cook
Preset oven Gas Mark 4, 180°C (350°F).
Put the garlic, ginger, lemon rind, parsley, mint and rosemary in a food processor. Switch on for a minute or two until everything is finely chopped. Switch on again and add the oil slowly until you have a bright green mixture. Set the mixture aside.
Place the joint in a roasting pan with the onion and water, cook, allowing 20-25 minutes per ½ kg (1 lb). Thirty minutes before the end of cooking time remove from the oven, spread the herby mixture over the joint. Return to the oven and finish cooking. Keep an eye on the water level. Top it up if necessary.
When the lamb is cooked remove from the pan and keep warm. Discard the onion and remove excess fat. Add a dash of wine to the pan juices. Boil up and reduce to a nice syrup. This will take 2-3 minutes. Season and serve with the sliced lamb.
One Portion (200g meat) = 8 protein exchanges
Check your diet sheet to see what your daily allowances is.
If you are in need of a sugar boost to keep up with all your chocolate eating friends you can try this very simple tray bake.
15’s
Serves: 20
 Ingredients
Ingredients
- 15 large marshmallows
- 15 digestive biscuits, crushed
- 15 glacé cherries, halved
- 150ml condensed sweetened milk
- 75g desiccated coconut
Method
- Cut the marshmallows in halves using scissors, and place in a large bowl. Toss with the digestive biscuits and candied cherries. Gradually stir in the sweetened condensed milk until the mixture becomes a soft, moist dough. It should not be too dry, so you may need to add a bit more milk.
- Spread a generous layer of coconut out on a clean surface, and place the dough on top of it. Use your hands to form the dough into a long thick sausage, making sure it is well coated with coconut. Wrap in a double layer of cling film, and refrigerate for 2 to 3 hours.
- Unwrap the long piece of dough, and cut into slices to serve.
This is a high fat and high sugar treat, so it may not be for you if you are watching your weight or diabetic.
Despite the springtime showers many people on dialysis have to limit the amount of fluid they drink each day. Complete the following crossword puzzle and find a few simple tricks to help quench your thirst while sticking to your fluid allowance.
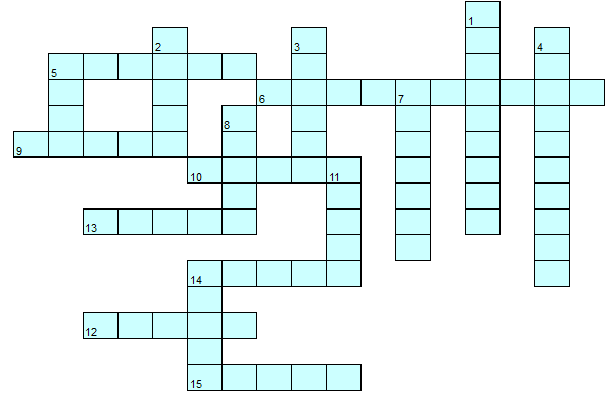
Across Down
5 Keep boiled EWSTES in the fridge. 1 Rinse your mouth with chilled WOTAMHSUH.
6 Try to take ONDEATMICI with 2 Keep track of how much you HIGWE between
with mealtime liquids. dialysis sessions.
9 SHUBR your teeth often. 3 EFZERE small pieces of fruit from your daily
10 Fill a container with the fruit allowance such as grapes.
recommended amount of TRAWE 4 If you are diabetic keep your GLUDBSOOAR
each morning & use this for the day. under control to reduce thirst.
12 When taking other fluid pour 5 Use OSRU sweets to moisten your mouth.
out an UQALE amount of water 7 GIWHCEN gum can help to reduce thirst
from the pre-measured container. 8 Keep a fluid YRIDA.
13 Avoid ATLSY foods. 11 ESNIR out your mouth with cold water.
14 When on holidays stay cool by 14 Use ALMSL cups and glasses.
staying in the EDAHS.
15 Use a OMELN slice to freshen your mouth.
Oonagh Smith. Renal Dietitian Beaumont Hospital
What’s sizzling this summer?
Written by Eamon Donovan on . Posted in Blog.
As the inclement summer season rolls on, the optimistic among us have our picnic baskets and barbecue tongs on standby. You can enjoy a fun filled summer picnic or barbecue by making wise food decisions. So when the sun does start to shine, be renal diet ready with our top tips and tasty recipes.
- For the barbecue, choose burgers, chicken, fish, steaks or pork chops. Fresh meats are low in salt compared to processed meats like hot dogs and sausages. At the picnic, choose fresh, unprocessed meats, poultry or fish for your sandwich fillings rather than ham, bacon, and smoked salmon which are high salt choices.
- Limit high potassium foods. Summer barbecues and picnics often contain large amounts of salads which are high in potassium e.g. tomato or potato salad.
- Monitor your fluid intake. Use a small glass. Remember to enjoy alcohol in moderation.
- Offer to make a side or main dish for the barbecue or picnic if you are not hosting it. You will be sure that there will be something tasty that you can eat.
Each recipe will tell you how many protein and vegetable exchanges a serving will provide. None of the recipes contain high quantities of dairy or potatoes and as such will not affect your daily allowance.
Check your diet sheet to see what your allowances are.
All the recipes are kidney friendly and do not include ingredients that are high in potassium, phosphate or salt. If they are low in fat they have been marked low fat. The allowances (exchanges) are in keeping with the Irish Nutrition & Dietetic Institute (INDI) renal diet sheet.
Egg mayonnaise and cress sandwiches
Serves 4
Ingredients:
4 medium, hard-boiled, peeled, chopped
3 tbsp mayonnaise
1 tsp ground black pepper
8 slices white bread, lightly buttered
¼ bunch cress
Method:
- For the egg mayonnaise and cress sandwiches, mix the eggs and mayonnaise together in a bowl. Season, to taste with freshly ground black pepper.
- Spread the egg mayonnaise onto four slices of the bread. Sprinkle over the cress and close the sandwiches with the remaining slices of bread.
- Remove the crusts and cut each sandwich into four small triangles.
Per portion: 1 sandwich (or 4 small triangles).
This dish provides 1 protein exchange.
Lemony Chicken Pittas
Serves 4
Ingredients:
12 butterhead lettuce leaves (60g)
8 slices cucumber (48g)
1 tbsp fresh mint
4 tbsp fresh lemon juice (80ml)
400g roast chicken breast
4 small white pitta breads
Method:
- Shred the lettuce and mix with some chopped cucumber, a pinch chopped fresh mint and the lemon juice.
- Chop the roast chicken into pieces and stir into the salad.
- Slit open the pitta breads and warm briefly in a toaster.
- Stuff pitta breads with the salad and chicken mix.
Per portion: 1 small round filled pitta. This dish provides 1/2 portion of vegetables and 3½ protein exchanges. This is a low fat dish.
Barbeque lamb kebabs
Serves 4 (8 skewers)
Ingredients:
400 g leg of lamb, cut into 1 inch cubes
1 red, 1 green pepper, stem and seeds removed and cut into 2.5 cm cubes
2 red onions peeled, quartered and divided again (16 pieces in total)
For the marinade
2 tbsp olive oil
Juice of half a lemon
1 garlic clove, crushed
You will also need 8 skewers. If you are using wooden skewers, soak them in water for 30 minutes prior to use. This helps to stop them from burning. If you are using metal skewers, take care as they will get very hot!
Method
Mix the ingredients for the marinade together in a bowl. Add the lamb, cover and leave to marinade in the fridge for at least 30 minutes.
Thread alternate pieces of lamb, pepper and onion onto your skewers to make approximately 8 kebabs
Cook on a hot bbq for 10-15 minutes, depending on how you like your lamb, turning regularly.
Serve with pitta bread.
If preferred or if the weather isn’t befitting a bbq, you can cook the kebabs on a grill or griddle pan.
Per portion: 2 kebabs provides 3 protein exchanges and 1 vegetable exchange
Beefburgers
Serves 4
Ingredients
- 450 g minced beef
- 1 onion, chopped
- 2 tsp mixed herbs
- 1 egg , beaten
- Freshly ground black pepper
To serve (to make 4 portions)
- 1 small red onion, sliced
- 1 tomato sliced
- 4 leaves ice berg lettuce
Method
Mix the ingredients for the burger together in a bowl.
Divide the mixture into 4 large or 8 small patties
Cook the burgers for approximately 15 minutes or until well cooked through
Serve with side salad as above and a burger bun or ciabatta roll as desired
Per portion: 1 beef burger with side salad provides 31/2 protein exchanges and 1 vegetable exchanges
Rice and pineapple salad
Serves 4
Ingredients
- 120 g long grain rice
- 1 yellow pepper, deseeded and finely chopped
- 3 spring onions, trimmed and finely chopped
- 3 rings of tinned pineapple
- 5 tablespoons French dressing
Method
Boil the rice until cooked, drain and allow to cool.
Once cooled, tip the rice into a bowl.
Add the pepper, pineapple, and pepper
Stir in the dressing and serve
Per portion: salad provides 1 vegetable exchanges
Joanne Walsh, Senior Clinical Nutritionist, St. James’s Hospital, Dublin.
Gillian Quinlan, Senior Dietitian, Mid Western Regional Hospital, Limerick
Enjoying the Summer Holidays on a renal diet
Written by Eamon Donovan on . Posted in Blog.
As the holidays draw ever nearer, food is constantly on my mind! What to cook, when to cook, how much to cook and of course trying to make everyone happy. And I don’t even have to worry about a renal diet! So to make life seem more manageable I try to make lists and do some of the food preparation in advance. While it’s never quite as smooth as I would like, I am always very happy when I am able to pull a quick meal out of the freezer or have all of my ingredients at hand!
The holidays can be challenging on a renal diet, especially when you’re eating at someone else’s home, in a hotel or B&B, and you aren’t certain what’s in the food you’re being served. Here are a few strategies you can use to make the holidays go a bit more smoothly.
- make a list (check it twice) of the meals you’ll be cooking and the ingredients you will need; this can save time and money
- offer to bring something and plan on a dish that is kidney-friendly that you know you enjoy
- ask about the menu in advance; if there’s something you aren’t sure about you can ask your dietitian before you go
- make it a “recipe potluck”; suggest everyone brings enough copies of the recipes for the items they bring to share. Everyone gets to take home new recipes (a great memento of a holiday get-together) and you get to scan all the recipes to make sure you know what you’re eating!
- watch your portions; keep servings small and avoid going back for seconds – eat slowly and join in the conversation!
- don’t be too polite; don’t feel you need to clean your plate or try some of everything, especially if the food doesn’t fit well into your kidney diet
- avoid the “extras”; condiments and sauces such as, gravies, pickles, olives, cheese, nuts other than peanuts(not salted) or cashews etc – all of these “extras” can be sources of salt, phosphorus, or potassium. See more suitable homemade recipes on the next page.
- avoid skipping meals; if you’re starving you will be much more likely to overeat!
Tips on dining out easier on a renal diet:
|
When you know you will be eating out for dinner, plan your breakfast and lunch at home accordingly. Cut back on serving sizes and foods high in sodium and potassium during the day. Call ahead or check their website to learn more about the menu and how the food is prepared. Choose a restaurant where it will be easiest to select foods best suited for your diet.
Restaurants where food is freshly prepared and made to order are the best choice. Eating at fast-food restaurants is not totally out of the question.
It does, however, take some thought and planning. Fast food restaurants tend to have pre-prepared components for their meals, and often these are pre-salted too. This can make it challenging modify the meals according to your needs. Though, they usually have nutritional analysis of their meals which can be useful when making the best choice from their range of meals.
We love a bit of sunshine here in Ireland, but unfortunately it does not come around very often! But when it does, there is nothing quite like sharing a BBQ with friends and family. Some BBQs meals have high salt or high phosphate content, not to mention risks of food borne bacteria. But this does not mean you should miss out on delicious tasty meals! Here is an appetising BBQ meal you could enjoy!
While you are waiting for the BBQ to get started …
Starter: Pesto Pasta salad (Serves 4)
Ingredients
- 600g Pasta twists
- 80g red pepper, chopped
- 40g fresh basil
- 3 tbsp olive oil
- 1tbsp white wine vinegar
- 10g crème fraiche
Method
- Add the pasta to boiled water and cook until tender. Drain the pasta into a bowl and allow to cool – keep the cooking water in a jug
- Add the basil, olive oil, white wine vinegar and crème fraiche into food processor and blitz until it is a smooth consistency. (If it looks too thick, add some cooking water from the pasta – this will help coat all the cooked pasta).
- To finish, add the chopped red pepper to the pasta and mix the pesto through until all the pasta is coated. Serve chilled.
| Per portion this starter dish provides a ½ vegetable portion. Check your daily allowance to see if you have enough remaining for this dish
|
The Main course : Pork Kebabs (Serves 4)
Ingredients
For Kebabs
- 1 medium (75g) red onion, peeled
- 1 medium (80g) green pepper, removed core & seeds
- 325g pork fillet, cut into 1inch cubes
- 1 tbsp of red wine, to brush on during cooking
For marinade
- 1 tbsp olive oil
- ½ level tsp ground cumin
- 1 tbsp honey
- 1 clove of garlic
- 1 tbsp of fresh rosemary, chopped
Method
- Place 8 wooden skewers in water to soak (this will prevent them burning). Mix all of the marinade ingredients together in a bowl, and then stir in the pork. Cover and leave this to marinade for 2-3hours in the fridge.
- Preheat barbecue for high heat.
- For the kebabs, cut the onion into 16 equal size pieces. Also cut the green pepper into 16 equal sized pieces.
- To construct the Pork Kebabs, remove the skewers from the water and the meat from the fridge to start treading the pieces onto the skewers. Start with a piece of the meat first, then red onion, then green pepper, and repeat this again, and end the skewer with another piece of pork (the pieces of meat at both ends keep the pieces secure)
- Lightly oil the barbecue cooking grate. Arrange skewers on the prepared barbecue. Cook for 15 to 20 minutes, brushing occasionally with red wine, until meat completely cooked through and juices run clear.
Per portion
|
Summer salad (Serves 4)
Ingredients
- 1½ desert bowls (125g) Cos lettuce, roughly chopped
- 25g red onion, finely chopped
- 50g raw runner beans
- 1 level tbsp fresh coriander, finely chopped
- 1 level tbsp fresh parsley, finely chopped
- 1 tbsp olive oil
- 2 tbsp fresh lemon juice
Method
- Mix all the ingredients in a large bowl and gently mix to coat the salad
| Per portion this dish provides 1 portion of vegetable from your daily allowance. Check your daily allowance to see if you have enough remaining for this dish Check your daily allowance to see if you have enough remaining for this dish Couscous (Serves 4)
Ingredients
Method
|
“Superfoods” and the Renal Diet
Written by Eamon Donovan on . Posted in Blog.
Over the last two decades there have been a lot of changes to the Irish diet, and many new foods have become popular. There has been a lot of advertising in recent years about the reported health benefits of these new foods, and also of so called ‘super foods’. As Renal dietitians we are frequently asked whether these foods are suitable for people on Renal Diets, and if there is actually any benefit to be got from them.
Below I have compiled a list of some of these new foods, what their benefit is, and whether they are suitable for those on a renal diet or not.
Reported Health Benefit:
Blueberries are reported to help prevent the development of cancer, cardiovascular disease and age-related illnesses through their anti-oxidant properties.
Is this True?
At present there is no evidence that blueberries are any more beneficial than any other berries or fruit in terms of cancer and cardiovascular disease prevention. Most of the studies reporting their health benefits have only been done in a laboratory setting and not done in humans.
They are still beneficial for other reasons as they provide important vitamins, minerals and fibre to the diet, however they are no different to any other fruit in this respect.
Are they Allowed on a Renal Diet:
Yes, but in moderation. Like all fruit blueberries are high in potassium so keep it to 100g (100 berries) or less a day as a portion, and make sure to include it as part of your overall daily fruit allowance. Blueberries contain sugar so if you have diabetes make sure to discuss it with your dietitian before taking them.

Chia Seeds
Chia Seeds are tiny edible seeds that come from a desert plant in Mexico. They are unprocessed wholegrain seeds that can be eaten whole and absorbed directly into the body, unlike some other seeds that must be ground first in order to be absorbed by the body.
Reported Health Benefit:
They are reported to help aid weight loss through controlling hunger.
Is this True?
In theory these seeds are meant to expand in your stomach, which in turn helps you feel full for longer and thus aid in weight loss. However actual evidence on chia seeds is limited and a review of the available studies found no evidence of any effect on weight loss.
Are they allowed on the Renal Diet?
These seeds are quite high in protein and phosphate, with a two tablespoon dose giving an average of 25-30% of your daily phosphate allowance. For this reason these seeds are not recommended for people on Renal diets.
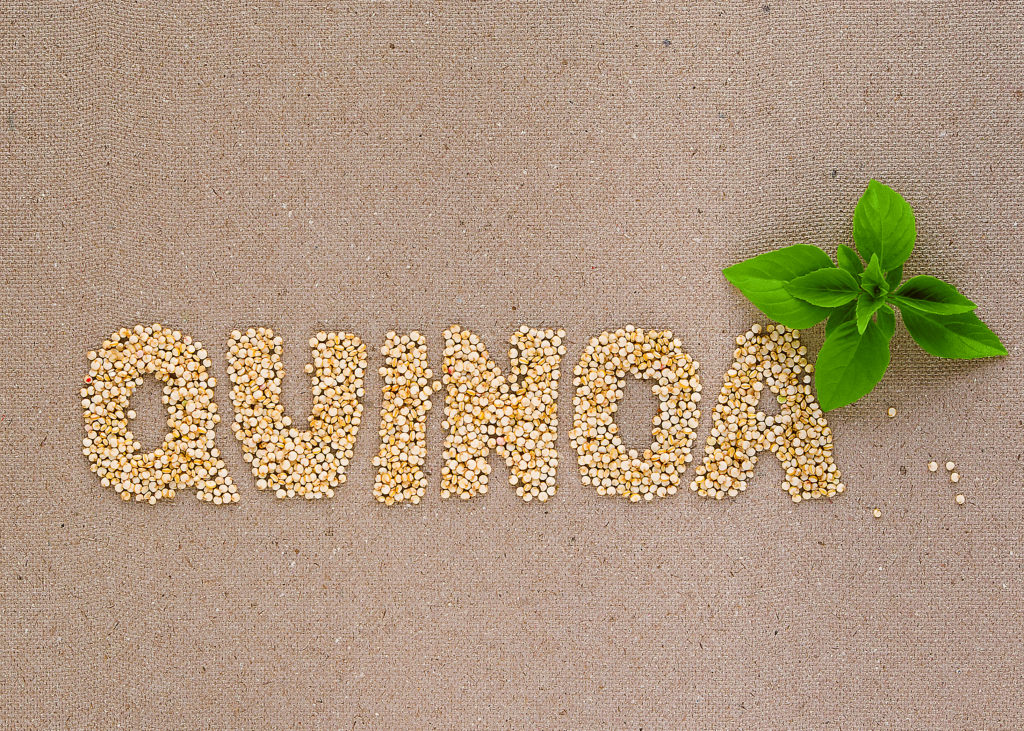
Quinoa
Quinoa has been grown in South America for thousands of years, and formed a staple part of the diet of the people native to that area. Although quinoa acts as a starchy food in dishes, it is actually a seed. It is therefore wheat free which is one of the reasons that it has gained popularity in recent years, as there are an increasing number of people following wheat free diets.
Reported Health Benefit:
It is wheat free and very high in protein, having double the protein content of rice or barley. It is also considered to be a ‘whole protein’, meaning that it contains all of the body’s essential amino acids; and is high in several minerals and B vitamins.
Is this true?
Yes quinoa is wheat free and a high protein source and is rich in Calcium, Magnesium, Phosphorous and Potassium.
Is it allowed on a Renal Diet?
Due to quinoa’s high potassium and phosphate content it should not routinely be taken by someone following a renal diet.

Wheatgrass
Wheatgrass is a type of grass and is a concentrated source of vitamin A, vitamin C, and vitamin E, iron, calcium, magnesium, and amino acids.
Reported Health Benefits:
Wheatgrass has numerous reported health benefits including lowering cholesterol, lowering blood pressure, helping to treat infections of the respiratory and urinary system and it is also used as an alternative health treatment in certain types of cancers.
Are these reported benefits true?
There is very little evidence that wheatgrass actually works to prevent disease or to detoxify the body in the way it is claimed. Of the studies published most of the numbers were too small to prove an actual beneficial effect from wheatgrass.
Is it allowed on a Renal diet?
Wheatgrass is usually taken as a juice and as such is very high in potassium; therefore it is not a suitable drink for people with kidney disease.

Cranberry Juice
Reported Health Benefits:
Cranberry juice is mostly commonly used in the prevention and treatment of Urinary Tract Infections (kidney/bladder infections).
Is this true?
Cranberry has been shown to be beneficial in the prevention of urinary tract infections as some of the chemicals in it prevent bacteria from sticking to the lining of the urinary tract. However it has not been proven to be beneficial in the treatment of urinary tract infections as these chemicals do not have the ability to release these bacteria once they have already stuck to the lining of the urinary tract.
Is Cranberry Juice allowed on a Renal Diet?
Yes, but in moderation. Like all fruits cranberries are high in potassium, therefore you should not have more than 200mls of cranberry juice per day. It must also be included as part of your daily fruit and vegetable allowance.

Acai Berries
Acai berries are a small reddish-purple fruits that comes from the acai palm tree, which is native to Central and South America. As these are a highly perishable fruit they can only be got in freeze dried form in Ireland.
Reported Health Benefit:
As they contain high levels of anti-oxidants, they are reported to have anti-aging effects and to aid in weight loss.
Is this True?
Like any fruit acai berries are full of vitamins, mineral and anti-oxidants, however so far studies have failed to show any conclusive health benefit in these berries over other similar fruits.
Are they allowed on a Renal Diet?
As it is only the freeze dried form that is available in Ireland, they are not suitable for those on a renal diet due to being very high in potassium. In fact the potassium content of 100g of these dried berries is equivalent to or higher than that of a banana.
The foods listed above are only a short list of some of the foods introduced to Ireland in recent years. If you have a new food that you would like to try and are following a Renal Diet always ask your dietitian if it is suitable first.
Mary Byrne, Renal Dietitian, Mater Misericordiae University Hospital.
Lemon Sole Meal Plan
Written by Eamon Donovan on . Posted in Blog.
This meal plan will suit those with advanced kidney disease. It provides 1980kcal and 63grams of protein. Please compare the full analysis and or Kidney Diet Allowances with your individual allowances. Your Kidney (Renal) Dietitian will help you to do this.
This 1 day meal plan provides 4 protein exchanges (allowances), 1 dairy exchange, 2 fruit portions, 2 vegetable portions and 2 potato portions. Check your daily allowances to see if you have enough for this meal-plan.
Total Nutritional Analysis
| 1980kcal | 63g protein | 75g fat | 5.2g salt | 54mmol / 2113mg Potassium | 30mmol / 919mg Phosphate | 280g Carbohydrate | 110g sugar |
Grilled Pork Meal Plan
Written by Eamon Donovan on . Posted in Blog.
This meal plan will suit those with advanced kidney disease or those who require a daily intake of 1586kcal and 57g protein. Please compare the full analysis and/or kidney diet allowances with your individual allowances. Your Kidney (Renal) Dietitian will help you to do this.
This 1 day meal plan provides 4 protein exchanges (allowances), 1 dairy exchange, 2 fruit portions, 2 vegetable portions and 2 potato portions. Check your daily allowances to see if you have enough for this meal-plan.
Total Nutritional Analysis
| 1586kcal | 57g protein | 65g fat | 3g salt | 49mmol / 1925mg Potassium | 762mg Phosphate | 200g Carbohydrate | 79g sugar |
[quote author=”Dietitian Tip” source=”” ]Ask your Kidney (Renal) Dietitian about a Low Phosphate Milk Substitute.
Watching your Fluid?
Remember to count your milk and milk substitute as part of your daily fluid intake.
[/quote]
*60ml milk substitute has been included in the analysis for this meal plan.
Lamb Chops with Redcurrant and Mint Sauce Meal Plan
Written by Eamon Donovan on . Posted in Blog.
This meal plan will suit those with advanced kidney disease or those who require a daily intake of 1738kcals and 64 g of protein. Please compare the full analysis and/ or Kidney Diet Allowances with your individual allowances. Your Kidney (Renal) Dietitian will help you to do this.
This 1 day meal plan provides 4 protein exchanges (allowances), 1 dairy exchange, 2 fruit portions, 2 vegetable portions and 2 potato portions. Check your daily allowances to see if you have enough for this meal-plan.
Total Nutritional Analysis
| 1738kcal | 64g protein | 67g fat | 4.2g salt | 55mmol / 2141mg Potassium | 877mg Phosphate | 231g Carbohydrate | 89g sugar |
[quote author=”Dietitian Tip” source=”” ]Ask your Kidney (Renal) Dietitian about a Low Phosphate Milk Substitute .
Watching your Fluid?
Remember to count your milk and milk substitute as part of your daily fluid intake.
[/quote]
*milk substitute has not been included in the analysis for this meal plan. Ask your Kidney (Renal) Dietitian about a milk substitute
Salt
Written by Eamon Donovan on . Posted in Blog.
‘A high salt intake holds onto water, increases blood pressure and increases thirst making it harder to follow your kidney diet and fluid restriction. The Kidney (Renal) Dietitians explain here why it is better to leave the salt in the sea!’
Salt or sodium chloride is needed in very small amounts in the body for maintaining water balance, healthy blood pressure and healthy muscles and nerves. However, too much salt in your kidney diet may lead to increased thirst, high blood pressure and cause your body to hold onto too much fluid. This extra fluid puts extra pressure on your heart to pump blood around your body, thus the more fluid you retain the higher your blood pressure will be. Increased thirst can make it difficult to maintain your fluid restriction.
Even without adding salt to your food, you can easily get more than you need by including processed foods that have a high salt content in your kidney diet. It can take up to six weeks for your taste buds to adjust to having less salt, but soon you should find that you are enjoying the real flavour of your food.
To reduce your salt intake:
- Avoid using salt at the table and if needed use only a pinch of salt in cooking.
- Choose fresh foods instead of processed and canned foods.
- Use herbs and spices instead of salt in cooking and at the table.
- Check food labels for the salt / sodium content to help make healthier choices.
It is important not to use salt substitutes such as Lo Salt and So-Low, as they are very high in potassium.
Avoid having the following foods as they contain large quantities of salt:
- Bacon, sausages, black and white puddings processed meats (corned beef, salami, pate)
- Frozen and take away meals, convenience foods, meals containing soy sauce.
- Smoked fish and fish pastes
- Tinned vegetables (unless marked ‘no added salt’)
- Tinned and packet soups, casserole mixes (e.g. Bovril, Oxo, Marmite), stock cubes
- Bottled canned and packet sauces and tomato juice
- Crisps, salted biscuits (e.g. Tuc, Ritz) and other salted snacks e.g. nuts and popcorn
- Keep to less than 100g (4oz) cheese a week. Refer to your individualised dairy allowance as provided by your Renal (kidney) Dietitian.
- Avoid salt substitutes.
Role of the Kidney
Written by Eamon Donovan on . Posted in Blog.
‘Measuring the size of a fist and located in your lower back, the kidneys are a hive of activity. Find out more about what kidneys do and what is kidney disease?’
What do kidneys do and what is kidney disease?
The kidneys are two bean shaped organs located in your lower back. Each kidney is about the size of a fist and weighs about 4-6oz. Inside the kidneys are tiny structural and functional units call nephrons which filter the blood.
The kidneys have many functions, including:
- Removal of wastes and excess fluids by cleaning and filtering the blood, and producing urine.
- Production of hormones which help maintain healthy bones, control blood pressure and control the production of red blood cells which carry oxygen around the body.
What is kidney failure?
Kidney failure may be described as a loss in the kidney’s ability to filter (remove) waste products from your blood. Kidney failure can happen quickly, caused by for example a sudden loss of large amounts of blood, or an accident and this is called acute kidney injury. Acute Kidney Injury is usually short lived, but can occasionally lead to lasting kidney damage. It may also be abbreviated to AKI.
More commonly, kidney function worsens over a number of years and this is called chronic kidney failure or chronic kidney disease (often abbreviated as CKD).The National Kidney Foundation state that up to two thirds of CKD is caused by uncontrolled diabetes or high blood pressure (hypertension). CKD is usually not reversible but if found early, progression can be delayed through medication, diet and lifestyle changes by maintaining current kidney function.
What is the definition of chronic kidney disease (CKD)?
Chronic kidney disease (CKD) is defined as the presence of kidney damage, or a decreased level of kidney function, for a period of three months or more.
Signs of kidney damage include:
- Persistent small and large proteins in the urine (proteinuria and microalbuminuria)
- Persistent blood in the urine (haematuria) – after exclusion of other causes, e.g. urological disease.
- Structural abnormalities of the kidneys demonstrated on ultrasound scanning or other radiological tests e.g. polycystic kidney disease, reflux nephropathy
- Biopsy proven chronic glomerulonephritis
The Irish Nephrology Society currently recommends classifying Chronic Kidney Disease into five stages based on a measure estimated glomerular filtration rate (eGFR).
Sometimes CKD can lead to end stage kidney disease, (eFGR)(ESKD) which requires dialysis or a transplant to keep you alive. However, as the Irish Nephrology Society (INS) state, ‘the vast majority of patients with mild to moderate CKD will not require dialysis and can be managed in primary care’. Early detection and treatment may help prevent ESKD and the need for dialysis or transplant treatment. The kidney diet is one of the cornerstones of the treatment of CKD and helps with the target of delaying progression. The kidney diet is also essential in maintaining quality of life and functional capacity in people with kidney disease. The type of kidney diet required is individualised to the stage of kidney disease (based on eGFR), other diseases present (co-morbidities), the person’s age, weight and social situation. Some examples of important kidney diet changes in the early stages of CKD are ‘A No Added Salt’, ‘Weight Reduction’ (if overweight) and ‘Moderate Protein Intake’. A Kidney (Renal) Dietitian can assess your diet needs and advise on a tailor made kidney (renal) diet.
How do I know if I have CKD?
Chronic kidney disease includes conditions that damage your kidneys and decrease their ability to keep you healthy by doing the jobs listed. If kidney disease gets worse, wastes can build to high levels in your blood and make you feel sick. You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. is sometimes called a silent disease because there are often no warning signs. Some signs of CKD are:
- Weight loss and poor appetite
- Swollen ankles, feet or hands (due to water retention)
- Shortness of breath
- Blood or protein in your urine
- An increased need to pass urine, particularly at night
- Itchy skin
- Muscle Cramps
- High blood pressure (hypertension)
- Nausea
- Erectile Dysfunction in men.
You often will not know if you have CKD as you may not experience any symptoms, however screening is based on simple urine and blood test that your doctor can easily perform. If you have high blood pressure or diabetes or you are obese, yearly screening should be considered with your doctor.
Remember! Early detection of CKD may allow you to delay progression through diet and lifestyle changes and medication.
- 1
- 2