Phosphate Additives and the Kidney Diet
‘Advice from the Kidney (Renal) Dietitians on the importance of avoiding food containing phosphate additives’
Phosphate additives are added to foods for many reasons. They can be used to extend shelf life, improve colour, enhance flavour, or retain moisture.
The phosphates in food additives are especially dangerous if you have kidney disease since our bodies absorb them much more efficiently than the phosphates that occur naturally in foods like dairy foods, lentils and whole-grains.
Unfortunately there is no complete list of all foods containing phosphate additives because there are too many of them. Some examples of processed foods which may contain these additives are listed below.
Processed meats, processed fish and cheese, dried foods, dessert and cake mixes, cola drinks, alcoholic beverages, salt substitutes, instant pasta, sauces and bakery products.
Many products marketed as “low sodium” contain high amounts of phosphate additives. Cold meats with phosphate additives may contain up to 70% more phosphates than brands containing no additives.
How to avoid phosphate additives in your Kidney Diet = Read the Labels
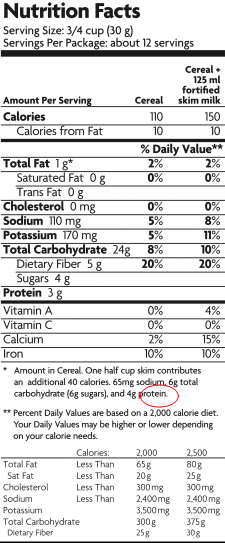
Reading labels is the key. Try to read the food labels of processed foods that you use regularly. Food additives are considered ingredients and must be listed in the ingredients list by specific name or designated E number.
The most common ones are listed below:
E338 Phosphoric acid
E339 Sodium phosphates
E340 Potassium phosphates
E341 Calcium phosphates
E343 Magnesium phosphates
E450 Diphosphates
E540 Dicalcium diphosphate
E541 Sodium aluminium phosphate
E542 Bone phosphate
E544 Calcium polyphosphates
E545 Ammonium polyphosphates
Foods containing these ingredients are best avoided on the Kidney (Renal) Diet.
Compare products and choose those without phosphate additives.
Look for foods labelled “free from artificial colours, flavours and preservatives”.
If you need help or advice ask your Kidney (Renal) Dietitian.